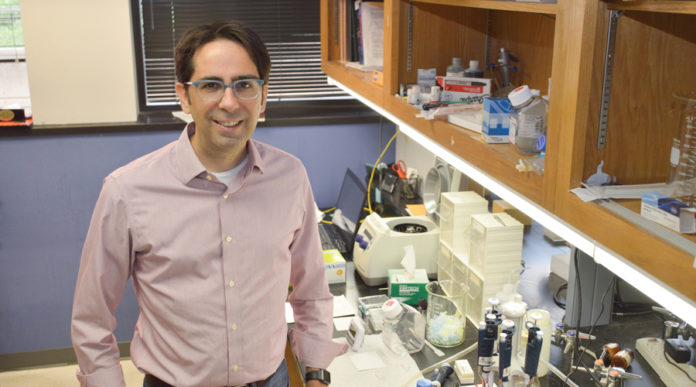
Ralph Shelton, Ph.D., of Perkins, lived with the effects of stress incontinence for more than five years following surgery for prostate cancer, until his physician, Ash Bowen, M.D., OU Medicine urologist, suggested the ProAct system.
According to the American Urological Association, between six and 20 percent of men continue to experience the life-disrupting impact of stress urinary incontinence a full year after prostatectomy. Approved by the Federal Drug Administration in 2017, the ProAct system is a device that addresses incontinence and restores quality of life for many men who deal with the challenges of this condition.
Late last year, Shelton was among the first Oklahoma to undergo the procedure to implant the ProAct system. “It’s a complete turnaround from where I was,” he said.
Bowen explained that urinary incontinence is a very distressing condition, an unfortunate but common consequence that occurs in connection with prostate surgeries, including radical prostatectomy or transurethral resection of the prostate. Physical movement or activity, from coughing or sneezing, to more vigorous activities such as running, lifting and other physical exertion, creates stress on the bladder. “When the muscles surrounding the bladder and urethra are damaged, that loss of muscular support causes incontinence, which may range in severity from very minor leaks to extreme – total loss of urinary control.”
The ProAct implantable device consists of two small, adjustable balloons, connected through short tubes to an injection port. Inserted on each side of the urethra during a short outpatient procedure, these fluid-filled balloons keep pressure on the bladder to help prevent urine leakage. The ports make it possible to adjust the pressure as needed to meet a patient’s individual needs.
The leakage Shelton lived with required the use of absorbent pads all the time. “It was embarrassing; there was always a risk when I went anywhere or tried to participate in any activity. Intimacy was awkward and less than confident,” he said.
Bowen said Shelton was a prime candidate for the surgery: he was doing well after prostatectomy, had no underlying health conditions, was physically active, and was ready and willing to find a solution to the incontinence problem he had endured for years.
The device has been widely used in Europe since 2002, and follow-up studies in the United States are promising for long-term (five years or more) benefits.
“The device is safe and effective,” Bowen said. “Potential complications are only what might be expected with any surgical procedure – risk of infection or reaction to anesthesia, for example. Side-effects encountered with the ProAct device are mild and easily managed.”
He cited a number of patient benefits related to the procedure itself. “The procedure typically takes only 30 minutes, is minimally invasive and is performed under general or local anesthesia in an out-patient setting – no hospitalization. There are no sutures or other anchoring devices. Most men experience only minor discomfort, if any.”
Shelton confirms that discomfort was minimal, and that the procedure was simple from the patient’s perspective. “I was back to my routine, daily activities quickly.”
If adjustments are needed, these also can be done non-surgically in an office setting. Shelton recently had one such adjustment with excellent results.
“Immediately after the procedure, I wasn’t sure there was much difference, but healing and recovery came quickly, and leakage began to decrease significantly. After one adjustment to increase the pressure, it works perfectly. It’s as if I never had a problem at all. I feel like I have my life back – I’m 100% normal.”
With a doctorate in adult education, Shelton taught generations of professional educators various techniques and methodologies to promote successful learning. In addition, he expanded his career, using his expertise to assess employer needs to ensure optimal hiring practices, matching a candidate’s skill set to the employer’s desired work objectives. He enjoyed ongoing opportunities to use these skills in retirement, until incontinence began to limit his activities.
Several years into retirement, he has no plans to resume an ambitious schedule of professional engagements, but the ProAct device does mean he can consider options that may not have been possible for him before the procedure. He continues to stay active and engaged in pursuits that use his well-honed skills of analysis. He currently works as a heavy equipment specialist for a local tractor dealership, once again using his expertise to assess needs and find solutions.
“Some may call it ‘odds and ends,’ but it’s still important to me to help people find ways to succeed. I’m something of a career-tech consultant, which offers me opportunities to travel, meet people and help facilitate a teamwork mentality. Now I know I can continue to do that that on my own terms, not limited by inconvenience or anxiety about accidental leakage.”
While a referral by a primary care provider is not considered necessary, it may be required for coverage under some healthcare plans. Bowen sees patients at OU Physicians Edmond, located in the Fountain Lake Center, 14101 N. Eastern, Suite E, and performs the ProAct procedure exclusively at OU Medical Center Edmond, One South Bryant. For an appointment, call (405) 340-1279.
www.crawfordcares.com