by Vickie Jenkins, Staff Writer
You’ve have heard the expression, every cloud has a silver lining, which means that even the worst events or situations have some positive aspect. The expression certainly can be said of the flight nurses that provide emergency medical services to numerous patients every year.
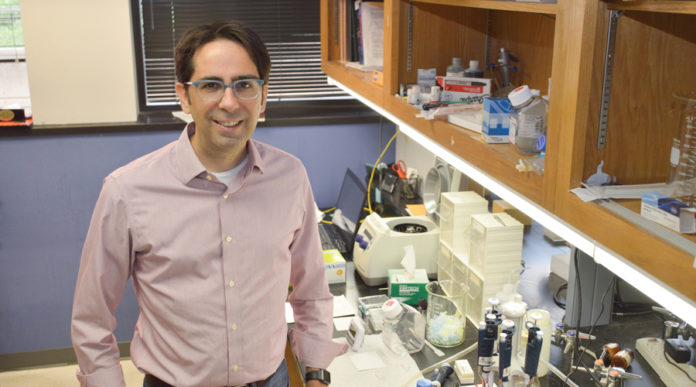
One outstanding gentleman is Matt George, RN, CEN, and the Medi Flight Clinical Base Supervisor at Medi Flight 5. “Medi Flight has been around since 1980. We are based on the helipad on the rooftop of Stillwater Medical Center in Stillwater, OK,” Matt said. “We leave from Stillwater and travel throughout central Oklahoma; largely around the Stillwater area, OKC, Tulsa and sometimes, Kansas. Our work also takes us to emergency situations in rural areas where they might not have the right emergency equipment.”
Matt attended Francis Tuttle for his LPN and Rose State college for his RN. It all began twenty-six years ago. “I always assumed that I would go into the medical field. I spent a lot of my time working in the emergency room, taking care of critically ill patients. My first job as a nurse was working in the medical surgical unit at Logan Medical Center in Guthrie, OK. I continued my education, becoming an RN. I realized I wanted to do more in the medical field and became interested in being a flight nurse,” he commented. “That was ten years ago and I will continue to do what I love to do; helping to save lives,” Matt added.
Matt explained the importance of a flight nurse. “On every flight, there are three of us; the pilot, a flight nurse and a paramedic. We work two twenty-four hour shifts and we always need to be ready to go! A typical day for me involves, making sure the medication count is correct, checking the medical equipment, talking with the pilot over issues of the day, looking over the aircraft and verifying that the helicopter is sound and ready for flight. We also need to pay close attention to the weather conditions; all three of us have our own little tasks to do but we all check the helicopter thoroughly. This is where teamwork is essential.”
What qualities make a good flight nurse? “I think the qualities for a flight nurse are the same for any nurse; they need to really care for others, doing what they like and wanting to continue to learn. Of course, to be a flight nurse, you would need to enjoy flying. Let’s face it, flying isn’t for everyone. Personally, I love it!” Matt replied.
Matt feels like his best quality as a nurse is caring for his patients. “I have always been drawn to the critically ill patients and it makes me feel good knowing that I am helping them. It is also some of the most interesting situations that I have even seen plus I am able to test my skills. Most flight nurses are required to have at least three years of experience in critical care and a high volume of life support service. The training for a flight nurse is constant and ongoing, testing once a year, making sure we are up to par,” he said. “I want to continue to learn and gain knowledge yet stay humble.”
Did you have any mentors in school? “Not so much in school but there were several nurses that I worked with that seemed to shape me into the kind of nurse that I am; helping me get situated and organized. They gave me a desire to learn and better myself,” Matt replied.
As far as Matt’s personal life goes, he is married to his beautiful wife, Shelly, and will soon be celebrating their twenty eighth wedding anniversary. They have two children, Kylee, 24 and Leah, 9 years old. “I am so proud of both of them,” he said with a smile. Their pet is an Alaskan Malamute. “His name is Sam,” he added. Matt’s hobbies include playing the guitar and singing. “I am an amateur guitar player and I sing a little, only at home and with my friends. Now, I did say amateur” he said with a laugh. “I also like going to the lake and boating. I do some home brewing too. With all of that, it keeps me pretty busy.”
If you were going to sum up your life in one word, what would it be? Without a pause, Matt said, “Fortunate.”