The Covid-19 pandemic has been a challenge to everyone. For many, the boredom and loneliness of staying home, away from family, friends and co-workers, has been the worst part. The members of the Edmond Quilt Guild have seen it as an opportunity to help their community.
Judy Elliott, EQG’s president, first received a request for cloth masks from a local hospital on March 20th. In early April, EQG board members shared instructions for face masks on the Guild’s website and spread an appeal via social media and emails to their members. By April 6th, they produced and distributed 266 masks to 6 different groups. By April 13, 1462 masks had been donated to 15 organizations. On May 3rd, the total was 2895. On May 17th, the count was up to 4225.
EQG has donated face masks to 22 organizations – mostly in Oklahoma but as far away as Texas and New York. They were donated to hospitals – OK Heart, OU, Mercy, St Anthony’s, and VA. They went to Edmond Fire and Police departments and Edmond Public Schools. Some masks went to churches, doctors’ offices, home health agencies, a Masonic Lodge, nursing homes, and the OKC Zoo Primate House.
Donated masks worn by staff at Bradford Village.
The masks were made by 66 members and 9 non-members. One member commented that making masks was like eating peanuts – Once you start, it’s hard to stop. Many noted that they had plenty of time and fabric and were happy to contribute both to the effort.
For more information about EQG and their community efforts – please see http://www.edmondquiltguild.us/
EQG’s Mask Making Marathon
Can insects transmit coronavirus?
It seems like every year around this time, a new insect-borne virus comes along. Fortunately, at this time, experts say no data exists to suggest Covid-19 can be transmitted by either mosquitoes or ticks.
“Although highly contagious, Covid-19 does not appear to be spread through blood like some other communicable illnesses,” said Oklahoma Medical Research Foundation immunologist Eliza Chakravarty, M.D. “And it’s the blood-borne transmission that allows insects to transmit diseases like West Nile and Lyme.”
Covid-19 and other coronaviruses like SARS and MERS are spread from person to person through tiny viral droplets, which pass from one person to another through mucus or saliva.
The virus also survives on some surfaces for significant periods, “which means you can infect yourself by touching an object and then putting your hand in your nose, mouth or eyes,” said OMRF President Stephen Prescott, M.D.
While much still remains unknown about Covid-19, said Prescott, there is no biological reason to suggest transmission through insects is a threat.
“That’s good news, but it’s not a ‘get out of jail free’ card,” said Chakravarty. “Other diseases spread by mosquitoes and ticks are still dangerous. They didn’t go away just because Covid-19 is dominating the news cycle.”
In Oklahoma, the most common insect-borne diseases are West Nile virus, which is spread by mosquitoes, and Rocky Mountain spotted fever, which ticks pass from animals to humans. The Oklahoma Department of Health also reports that tick-borne Lyme disease may be present in the state.
“Oklahoma has a quite a few insect-borne diseases, and others like dengue and chikungunya could be on the way,” said Prescott. “These can result in serious damage to health, so it’s important we guard against them as temperatures warm and insect populations surge.”
If you’re practicing social distancing by gardening, walking the dog or reading a book on the patio, the best defense is to keep insects off your skin by wearing long sleeves and pants. Limit outdoor activities around dusk and dawn or walking though tall grass, and avoid excess standing water that collects in flower pots, gutters and drains.
Chakravarty also recommends applying an insect repellant that contains DEET.
“And, no, using DEET is not the threat some make it out to be,” said Chakravarty. “The amounts used in regular application pose no proven health issues. The real risk is getting bitten by an infected insect, because one bad bug bite can change your life.”
Stephenson Cancer Center Patient Keeps Hope Alive on Clinical Trial

On a wall in her home, Deborrah Winters hung a sign that perfectly captures her journey with cancer: This girl won’t stop.
Winters indeed has not stopped. A patient for nearly three years at Stephenson Cancer Center at OU Medicine, Winters has experienced numerous highs and lows. Her original tumor was successfully treated, only to return in a different part of her body. Through it all, she remains determined to fight cancer alongside the healthcare providers that she considers her teammates in the effort.
“I wouldn’t be here without the Stephenson Cancer Center,” said Winters, a Midwest City resident. “They fight WITH me. You don’t take this journey on your own. They go the extra mile – they don’t just treat what’s going on in your body, but they treat your body, mind and spirit. Nobody has given up on me.”
Winters’ battle against cancer began in October 2017, when she was experiencing abnormal bleeding. She was quickly referred to Stephenson Cancer Center, where she was diagnosed with stage four uterine cancer and learned that a tumor the size of a baby’s head had begun bleeding. She started treatment immediately but soon faced another hurdle — a stroke. After being hospitalized, she recovered.
However, her initial treatment for cancer wasn’t working, so she was switched to another treatment, which was successful beyond anyone’s expectations.
“It was just supposed to shrink my tumor enough to give me a longer life and better quality of life. But my tumor shrank and shrank until it floated away to nothingness,” she said. “It was awesome.”
But the good news didn’t last. During a regular CT scan last summer, doctors found that the cancer had returned, but in a different area – her intestinal tract. That’s when she was enrolled in a phase 1 clinical trial and began taking a targeted therapy matched to her tumor profile, said Kathleen Moore, M.D., director of the Oklahoma TSET Phase 1 Program and Associate Director for Clinical Research at Stephenson Cancer Center. Winters’ cancer has had a complete response to the therapy and she remains on the trial, Moore said.
Receiving treatment on a clinical trial has not only controlled her cancer, but it has given Winters an opportunity to play a role in the advancement of cancer care. That’s something she takes seriously.
“I’ve told the clinical trial team that I want them to do all the tests they need to do to learn about my cancer and the treatment I’m receiving,” Winters said. “I want them to understand what’s working with me so that it can work on other people with cancer.”
Winters still faces a future in which her cancer could recur, perhaps in another part of her body. She said she views it not as a fight that she finishes, but one that she continues. And as the sign on her wall reminds her, “This girl won’t stop.”
“So many people have been on this journey with me – my family, my church family, people I don’t even know who are praying for me. And, of course, Stephenson Cancer Center,” she said. “They have talked me through everything – every test they’ve done and every drug I’ve taken. They go the extra mile to make sure I understand everything that is going on. They go above and beyond to make sure they are taking good care of me.”
THE FISH BOWL TOURNAMENT – $10,000 First Place Bass
For a second year, The Toby Keith Foundation will be hosting The Fish Bowl at Lake Texoma on June 20, 2020. First place in the Bass division is $10,000 (based on 150 boats) and a $500 prize goes to the worst fishermen. “We are aware that many nonprofits have had to cancel their fundraising events during the COVID-19 pandemic and we’re no different,” said Juliet Nees-Bright, executive director of The Toby Keith Foundation. She added that they have also pushed back their largest annual fundraiser, The Toby Keith & Friends golf tournament to October 17, 2020. “We are beyond grateful and excited to have found ways to revise The Fish Bowl to ensure everyone’s safety and keep it on our schedule,” added Nees-Bright.
The Foundation’s goal is to keep the momentum of this event going through a difficult time and do everything in their power to keep the fishermen safe while they enjoy the tournament. The Captains meeting will not be mandatory this year and will only be for those who did not register online or send in their registration via mail. Another major safety measure includes a drive-thru weigh-in. Both the Captains meeting and weigh-in will be held at Rally Pavilion, Rooster Creek. Online registration is open until 6 p.m. on June 19th at https://www.tobykeithfoundation.org/news-events/. If you send in your entry by mail after June 1st, please contact the foundation office at (405) 271-6552 to confirm that they’ve received your paperwork. Proceeds from the event benefit OK Kids Korral, a cost-free home for children battling cancer. Hundreds of children from across Oklahoma and surrounding states have stayed at OK Kids Korral while they are receiving cancer treatments. If you would like to know more about OK Kids Korral, please visit www.tobykeithfoundation.org.
“We are so grateful to the companies who supported us our first year and who have already signed on again this year amidst COVID-19,” said Nees-Bright. “Our sponsors are part of our family and they truly care about our Korral kids who are battling cancer.” Title sponsor is Precision Construction out of Oklahoma City and Florida. Other sponsors who signed on for a second year are: Bank7, AFR Insurance, Future Bass Team Trail, Vernon Auto Group and Keystone Broadcasting. The newest sponsorship addition growing the event is Applied Industrial Machining.
For more information about the event or to become a sponsor, call The Toby Keith Foundation at (405) 271-6552 or visit https://www.tobykeithfoundation.org/news-events/.
Diane Martinez – Life-long Learner and SCSEP Participant
Diane Martinez is the picture of a resilient journey through difficulties to success. As a Creek Indian and member of the Muscogee (Creek) Nation, her traditions are very important to her. She attends the Weoguf-kee (Muddy Waters) Ceremonial Grounds in Hanna, Oklahoma. Diane has learned some of her native Mvskoke language through classes at the College of the Muscogee Nation and tries to teach her grandchildren. She has survived many challenges and found a place where she can thrive. As a participant in the National Indian Council on Aging’s Senior Community Service Employment Program (SCSEP), Diane now works 20 – 30 hours per week to supplement her company retirement income. She has found a place with NICOA SCSEP to grow and learn additional employment skills.
Life was not always rosy for Diane. In 2014 at the age of 57, Diane resigned from her job. As time drifted forward, she felt more and more useless. The lumbering days lacked purpose. Being without a regular wage, she felt aimless and soon struggled financially. What seemed like a good idea, soon began to impact Diane’s goals and dreams. Emotionally, the lack of purpose and financial security was taking a toll on her wellbeing.
Diane states went through a period of being homeless and living in a shelter. She felt depressed and without hope. About this period, she states, “I knew and believed there was no hope for me.” She declares that she felt like meaningful employment was beyond her – “having gray hair and no teeth and being an older person.”
Working three different jobs over a four-year period and trying to live on a small pension, as well as income from baking goods and making jewelry, Diane moved to different places and stayed with different people. She lived with many relatives, but she kept a desire to have a stable income and to get into her own place. Diane suffers with back problems and arthritis. So, doing the physical work of the past was not very conducive to good bodily or mental health. Her decision to resign from a job she performed for 27 years was turning into a terribly difficult journey.
In 2019 Diane heard about the SCSEP program through a friend who was in the program in Okmulgee, Oklahoma. Her decision to apply for SCSEP has led her to definite changes. “When I called NICOA to see what they were all about I had no clue. I now know that NICOA SCSEP helps me to plan, have guidance, set goals, and believe in myself.” Working in the NICOA Central Region office as a receptionist trainee, Diane is gaining valuable skills that impact her opportunities for future unsubsidized employment.
“I am still able to work, and now I am becoming independent with more knowledge and wisdom. Through this program, I learned to be mindful and to help others like I was helped.” Through the SCSEP on-the-job training Diane states that she has “been spared and given an opportunity.” As a result of her own hard work, she has gained what she so often desired in her heart, a home and the skills to take care of herself financially, physically, and mentally. “I am grateful, and I appreciate this program.”
Diane’s goals and interests for her future include both employment and traditional aspirations. She has in mind to return to work fulltime in a clerical position. She wants to work five to ten more years and to continue to be independent. Diane hopes to stay connected to family, being surrounded by her grandkids. As important as these goals are, she hopes equally to continue to be connected to her Mvskoke-Muscogee culture through language learning, dances and traditional ceremonies. To her this will be a sound life and a demonstration to her family of how to age well as an elder. NICOA SCSEP is contributing as a valuable resource along this part of her journey.
RN’s First Love to Last Love – Editor’s Note: As part of the American Nurses Association “Year of the Nurse” campaign, National Nurses Month begins May 1st. During This very difficult time and in support of Oklahoma Nurses – we have devoted a large portion of our publication to nurses throughout the state. Please join us in saying THANKS!
story and photo by Vickie Jenkins, Staff Writer
Growing up in Holdenville, OK in the late sixties, people considered this as golden town living; a safe place to live, small in size and friendly folks. At the tender age of twelve, Barbara McDougal was like most girls, beginning to notice those once dreaded species called boys. She began to push her childish ways to the side, knowing that she would soon be a teenager. Barbara took notice of a certain boy that had just moved to the neighborhood, only one block away from her. She peeked out the window each time he walked by her house as he adventured out, exploring the mighty streets in the neighborhood.
As Barbara and her girlfriends gathered, Barbara found herself secretly pointing this boy out, telling them how cute he was, along with a firm statement of, “Someday, that boy is going to be mine.”
It wasn’t long before Barbara became more interested in this new boy in town. She would casually be sitting on the front porch at the most convenient planned out times. It wasn’t long before this boy walked by her house, stopping to introduce himself. It was just like one of those love stories on the big screen; the two of them stood there, gazing into each other’s eyes, as though a light suddenly came on. They knew the love bug had gotten to both of them. They had been love-struck!
His name was Bobby Aldridge and he was sixteen-year- old. He drove around town in his blue ‘57 Chevy and Barbara remembers the car being far out! After a few visits between the families and getting to know each other a little better, Barbara was allowed to meet Bobby for lunch at the local Dairy Queen. They spent their time holding hands as they listened to the juke box play some of their favorite music; Donavan’s Hurdy Gurdy Man and Tommy James and the Shondells. Soon, the relationship between the two of them progressed and they were inseparable!
In this time and age, when a boy liked a girl, he gave her a token of his love by giving her a drop, a necklace with the boy’s initials on it; Bobby’s initials being RLA. Now, they were going steady! The relationship between Barbara and Bobby was going perfect!
It was in 1970, that Barbara got the news that Bobby and his family were moving from Holdenville, to Oklahoma City, OK. No, this couldn’t happen! Both families hated to see the sweet couple separate but it had to be. Bobby’s dad had taken on a new job in Oklahoma City, OK. After the move, frequent visits were made by Barbara as her parents would drive to OKC, allowing Barbara to spend as much time as possible with Bobby. Little did they know that their relationship would be coming to an end in the near future.
Life brings changes when we least expect it and our paths take off in different directions.
Barbara graduated in 1974 and attended Oklahoma State University. This was a whole new world for her; college, new friends and discoveries of being an adult. Barbara became an LPN in 1978, working in Stillwater, OKC and even moved to Dallas, Texas for a while. Barbara realized that she needed to go back to school for her RN. She moved back to OKC in 2007 to begin RN school at OSU/OKC.
Time moves on. Barbara had just finished one of her classes and decided to go a near-by restaurant for lunch. As she sat at a booth, she noticed a gentleman sitting at a booth, across the room, not far from her. Taking a second look, he looked very familiar. Was it Bobby? With a feeling of nervousness and a little flushed, she got up and walked over to him. Yes, it was Bobby! They enjoyed talking to each other and reminisced about old times. Their love story picked up where they left off.
Barbara and Bobby were married on October 7, 2017. Barbara wore his initials, RLA as a charm on her charm bracelet in their wedding. This was the something old for her wedding.
Now, it’s the year 2020. Bobby is a homebuilder in OKC and Barbara is an RN at Mercy Rehab Hospital. Today, they still hold hands as they listen to some of their favorite music; Donavan’s Hurdy Gurdy Man and Tommy James and the Shondells.
From first love to last love, fifty-one years later and the love is still growing.
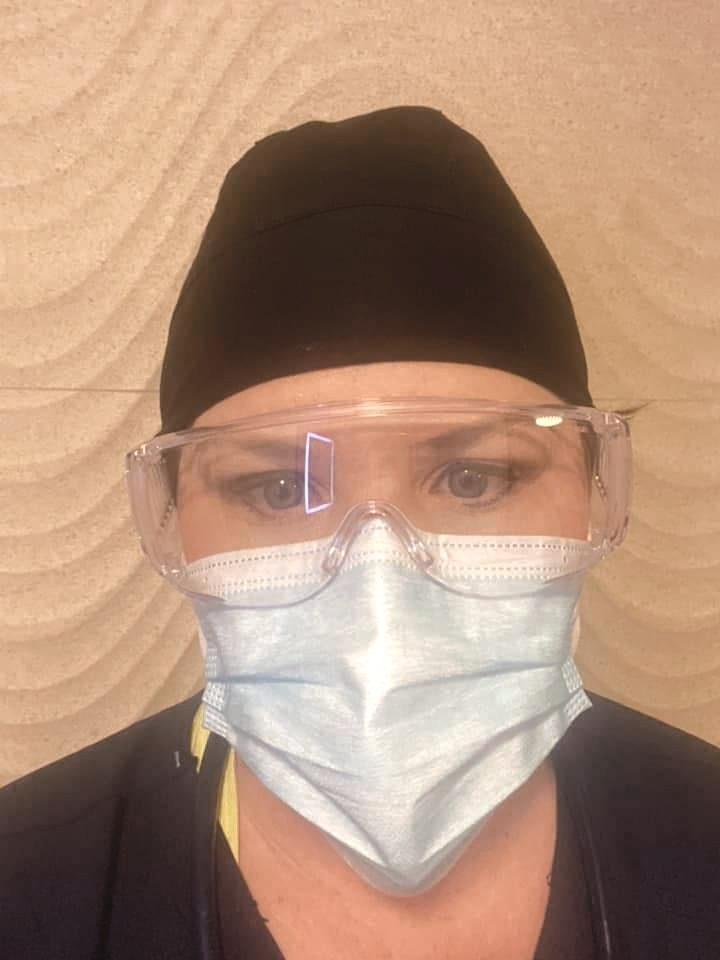
Behind the Mask: A nurse’s view

story and photo by Bobby Anderson, Staff Writer
At the time, none of us knew.
The patient we received from the emergency room was breathing 40-50 times a minute and maxed out on oxygen.
The bipap – the last line of oxygenation before a ventilator – wasn’t keeping up and the patient was struggling.
We knew the Coronavirus – or more technically, Covid-19 – was a thing.
Like all hospitals around us, there were whispers of a handful of patients on our campus being tested for it.
But they were in the ICU or on a separate floor, being taken care of by nurses with special personal protective equipment, wearing helmets and facemasks with powered air-purifying respirators.
Meanwhile, our patient was in respiratory distress.
Lab tests, chest x-rays and CT scans were reviewed along with a late call about the patient’s history.
The situation called for an ICU level of care.
The call from the patient’s doctor revealed COVID 19 was highly suspected.
That’s when COVID-19 became real for all of us in the room.
Outside the room, five respiratory therapists, the house supervisor and my charge nurse huddled together.
Eyebrows and voices raised.
The people I looked to most in the hospital for answers were without them.
Not only that, they were scared.
The bipap ventilation system was effectively aerosolizing the already contagious virus.
In layman’s terms, the high pressure flow made the viral particles even smaller and easier to transmit.
The surgical masks we were all wearing aren’t designed to be effective against the virus.
Two days later we learned the patient died while on a ventilator.
The day after that we learned results were positive for COVID-19.
Direct exposure was declared and all of us barred from returning to work for 14 days.
Nearly two weeks later we’re still learning.
Now I take my temperature twice a day and monitor for symptoms while logging everything online.
A fever over 100 degrees. A cough. Vomiting and diarrhea. Body aches.
All are symptoms of infection.
I haven’t been tested nor will I be tested unless I develop symptoms.
But my goal throughout this pandemic isn’t to complain or blame others. My goal, when I’m not at the bedside after my quarantine ends, is to highlight individuals who are helping turn the tide.
One of those individuals making a difference is Becky Lewis.
Lewis RN, MSN, CIC, is the system director of infection prevention for INTEGRIS, Oklahoma’s largest health system.
This virus has affected us all in different ways: personally, professionally and emotionally.
In Becky’s own words:
I see my family less and work more.
It is necessary but it is hard.
My five-year-old asks me when the sickness will be gone and my almost two-year-old cries when I come home because he knows that means it’s time to go to bed.
I come home and immediately start looking at any new common guidance documents from the CDC and the like to see if there were any revisions or updates overnight.
Every day I identify three to five items to focus on and work toward providing recommendations or guidance for each and relay that information to the system. The amount of updated or new information to digest is astounding.
I am currently on day 49 of non-stop COVID work. I am tired to my bones but know what I am doing is necessary and important work. I am working to keep our patients and caregivers safe.
I worry about the fear factor for our teams on the front line and the misinformation that can feel stronger than science.
My first week on the job as an infection preventionist was during H1N1 and it was wild, but we didn’t have the same social media presence that we do now and it is a strong element to work with and around.
One Pandemic — Two Brutal Outcomes
Story and photos by Darl DeVault
While Oklahoma seniors have been the most vulnerable to COVID-19, our modern heroes, medical health professionals, have also been impacted by this huge stress event.
Medical outcomes are stark. There are no proven therapies to treat or cure the disease. In Oklahoma, the vast majority of COVID-19 deaths are in seniors 65 or older, as high as 80 percent. The statistics go on and on, unchanging in dire descriptions of how vulnerable aging bodies are to the pandemic.
Another group shares a vulnerability every bit as brutal in descriptions. Our medical health professionals are the next highest death rate in America. Besides the brutal numbers of deaths, there is another facet of their suffering.
They are repeatedly exposed to preventable unmanageable stress. This immersion in the onslaught of a pandemic has the potential to inflict post- traumatic stress disorder.
In honor of the 200th birth anniversary of Florence Nightingale, the World Health Organization (WHO) has designated 2020 as the “Year of the Nurse and Midwife.” Since National Nurses Week is celebrated soon from May 6 through May 12 it is appropriate to ask one “What are you going through?”
Nurse Beth Bierig said last week from New Jersey, “Working on a floor of all COVID-19 positive patients whose change in status happens quickly without warning, makes you feel constantly guarded as to when your own medical health will quickly turn badly as well. You don’t have time to even comprehend how scary the silent killer surrounds every piece of air you work in, but it weighs heavily on your mind.”
Bierig, from Hackensack University Medical Center, goes on to explain how having a servant’s heart can put a nurse in harm’s way. “While performing life sustaining measures on your patients and respiratory fragments flood the air in the process, you can’t help but wonder, will it be saving their life that takes mine?” she said. “I don’t know the effects it will have on myself or other people, because everyone has had different experiences. Every nursing specialty has their own traumas and people are generally drawn to what they can handle.”
Also, “the support nurses receive after this will affect their long-term mental health pertaining to this situation. The whole situation has affected everyone strongly, not only health care providers. We’re living in a historic time and hopefully we all learn from it.”
From the respiratory therapists who manage ventilators, and technicians that manage ICU equipment to the direct caregivers, stress can be overwhelming. The heroes who share their servant’s heart signed up to be properly supported and use their knowledge and ability to affect positive change. Again, at present, there are no proven therapies to cure COVID-19.
Some health care professionals function where they are overwhelmed by the sheer number of deaths that take place right in front of them. Sometimes as often as hourly, these deaths may inflict a PTSD future on the frontlines of medicine.
For those healers who were constantly worried about their own health because of a shortage of personal protective equipment life can change. Just the apprehension of spreading the disease to their family could have a dire outcome.
COVID-19, the severe respiratory illness caused by the novel coronavirus pandemic is extremely transmissible. Properly protected ICU critical care team workers being readied for patient interaction look like preflight prep before blastoff for our moon missions.
These heroes may share an almost as strong an impact as the vulnerable seniors who perished. Some may suffer grave symptoms of psychological stress impacting their ability to deliver medical health care in the future.
Every psyche is different in the many roles played by helping healers who suited up to sustain the COVID-19 patients. Science tells us women are twice as likely to suffer PTSD symptoms.
This pandemic is something different. The onslaught of stress can change brain wiring for the worse — at the level to create PTSD. Later, some may seek to stay away from the situations that remind them of the traumatic events.
Some caregivers may not be able to adaptively overcome the stress and adversity while maintaining normal psychological and physical functioning.
The potential for PTSD is when an individual is placed in a situation where they do not have all the needed equipment, weaponry, support by colleagues in numbers needed, or proper support from superiors. This is also fueled when they feel they do not have the proper protective material and are forced to go in harm’s way relentlessly when they fear for their own survival. On April 3, Oklahoma showed 10.6 percent of its confirmed cases were health care workers.
Situationally produced and yet self-imposed is the stress of sleeping in their cars in their hospital parking lot because they do not want to bring potential illness and death home to their families. This can result in the development of PTSD, depression and other psychiatric disorders.
In a medical scenario where our heroes ran toward the danger and healing is supposed to take place that sounds extremely abrupt. But in many of our hospitals that were overwhelmed by COVID-19 patients presenting repeated unmanageable stressors, that is exactly what was happening.
Often nurses and doctors in COVID-19 hotspots made life and death choices, deciding who was to live and who was to die because of a limited number of ventilators and limited ability to intubate. And there was the randomness of patients dying right in front of them as these patients first entered the hospital.
We must be honest. Nurses and doctors are human and cannot escape that negative impact. People who signed up to work around the sick also take great pride in learning all the ways to be healers.
To suddenly be immersed in the onslaught of hourly and daily negative scenario can have a permanently deleterious effect on the human psyche. It remains to be seen if overwhelming the individual at a high morbidity level has a lasting effect. We know brainwave activity that negativity establishes can create specific pathways in the brain that were not there before.
How do we know what effect this has on these brave people’s body and spirit when these pathways are never compensated for? These individuals may have anxiety and depression from these days forward.
The wild card in all of this are brave medical health professionals who contracted COVID-19 themselves, while trying their best to help others. Hundreds have died around the world. Yes, they signed up for this profession, but not to suffer the same as their patients.
Another stressor is some hospitals, such as the University of Oklahoma Medical Center, are cutting pay and hours because of the strict emphasis on COVID-19 leaving them cash poor.
“A grateful nation will likely create a fund offering therapy and treatment for front line medical professionals who have health problems traceable to saving lives similar to the federal World Trade Center Health Program,” Oklahoman Kara De La Pena, APRN, said. “Considering for many of us who took on preventable risks, the James Zadroga 9/11 Health and Compensation Act of 2010 will be held up as a model for providing us medical treatment. That program is funded through 2090 now.”
The seniors saved and whole world thank our heroes and seek restorative insight into the medical outcomes thrust upon the healers who fight to keep people alive.
Guardian Angels Concierge service in trying times
by Bobby Anderson, Staff Writer
Social distancing. Infection risk. Quarantines.
The news during this pandemic has been enough to make your head spin.
Fear has been prominent no matter who you listen to and nearly everyone agrees – at least for now – it’s probably a good idea to just stay home.
For more than 30 years, Diana Hendrix worked in nursing home administration. She understands that life does go on and she also understands vulnerable populations.
That’s why six years ago she started Guardian Angels Concierge Service.
Little did she know that her business one day would be saving lives.
“Most of my seniors are pretty concerned. They don’t want to get sick,” she said. “They don’t understand why all this is happening but they still don’t want to get sick and don’t want their families to get sick.”
That’s where Guardian Angels comes in, to provide essential services during this time. Grocery shopping, light housekeeping and cooking still remain essential and Hendrix and her staff are able to provide those services.
”The one thing I’m trying to get out there is don’t be afraid to call us. Just because this is happening in the world if you need help call us,” Hendrix said. “I can do a certain amount of interviewing on the phone and pulling things together without actually being with a client. But even when I do have to see a client we’re very protective.”
In business since 2014, Hendrix brings her healthcare administration experience to her clients.
“I thought there would be a better way to help our seniors but I didn’t want to do any nursing. There are plenty of nurses out there and home health agencies. So I started out grocery shopping and making sure seniors ate and took their medicine.”
Grocery shopping and cooking was the easy part of.
Per regulations, Hendrix isn’t allowed to administer medication to clients but she can be there to remind her patients when they’re due.
The big thing I try to do for every family is try to find a solution for whatever is going on in their life,” Hendrix said.
As most non-essential stores have closed, errands are fewer for Hendrix.
“We’re still doing a lot of cooking which we do a lot of breakfasts, sandwiches for lunch and we do a great deal of crockpot and casserole cooking so clients can have them several days,” Hendrix said.
Hendrix and her staff are still able to still walk pets and provide other services just on a limited basis.
“We’re not taking any of our furry friends to the vet right now,” she said. “The vet I use is saying unless it’s an emergency we’re not really going into the vets.”
Another service is escorting patients to doctor’s appointments, which has taken on a new look.
“What they’re doing is they’re saying stay in your car and we’ll call you when the doctor is ready to see you,” Hendrix said. “They’re saying the fewer the better. They’ll take my client’s temperature, escort them into the doctor’s office and turn around and bring them back to the car.”
“They’re not wanting people to be in the waiting room at all.”
Things may look different but Hendrix and her staff are getting things done in this new normal.
“We’re trying our hardest not to go to stores. We’re doing as much as we can online,” said Hendrix.
Shoe coverings are donned before going into a client’s homes as well as gloves and sanitizing wipes.
Right now, the largest service is Hendrix is fulfilling is home organization including down-size packing. Regular housekeeping and laundry is also offered.
“When I started to look at the governor’s list to see if we were necessary,” she said. “The reason we fell into that essential spot was that if we didn’t come the client would not be able to do it. Picking up a load of laundry is hard for clients who use a walker or wheelchair. Making their bed, running a vacuum cleaner are things they need help with to stay at home.”
As the quarantine wanes on, Hendrix has noted her regular clients call more often.
But Hendrix and her staff are still there and talking with clients and reminiscing with them, brighten their days as they go along.
“It’s amazing I’m talking to them almost every day and I’m telling my staff to make sure you give them a call,” Hendrix said. “Those that started out with me … they’re still calling me.”
“I commend every administrator out there because I know they have a hard job.”
You can find out more about Guardian Angels online at guardianangelsokc.com or on Facebook.
Calm during the storm – Interim stands tall during crisis

by Bobby Anderson, Staff Writer
Now, more than ever, people need quality care at home from providers who can make sense of a daily changing healthcare environment.
For more than 50 years, people have turned to Interim HealthCare for that quality, compassionate care.
Ashley Simms, LPN, has been with Interim for two of those years, serving now as the assistant manager of sales operations.
“We realize for seniors and those with serious underlying health conditions home is the best place for them to be during this time,” Simms said.
While state and local governments mandate people stay at home to flatten the curve on Covid-19, care is needed more than ever inside the home.
“I think at this time it’s so critical … because legislatively there’s a lot of focus on hospitals which is important but these patients are going to come home and somebody has to take care of them,” Simms said. “There are so many factors that go into Covid that many people don’t consider such as fear and mental health.”
Interim HealthCare offers a full suite of services including: home healthcare, hospice care, personal care and support, veteran and spouse care, palliative care, behavioral health as well as neonatal and pediatric home care.
Interim offers services in Canadian, Cleveland, Grady, Kingfisher, Lincoln, Logan, McClain, Oklahoma, Payne and Pottawatomie counties.
The care extends beyond medical.
“Our social workers work diligently to help assist patients in obtaining necessary and basic items such as food and shelter which helps to drive down fear for our patients, especially in a time of crisis like this,” Simms said.
For several years, healthcare delivery has been trending more and more to a home setting to help curb rising medical costs. That means patients are coming home quicker and sicker than they ever have before.
And the hospital penalties for patients who readmit for the same diagnosis within 30 days can be substantial.
That’s why hospitals and other facilities rely on providers like Interim to stand in the gap and make sure patients safely recover at home.
With Covid-19 forcing more and more Oklahomans to stay at home, monitoring these high risk patients and intervening before they become sick has taken on an even greater importance.
Simms said Interim has long provided telehealth options for patients for daily monitoring of things like blood pressure, oxygen saturation and weight.
“A lot of times that provides calm to those patients because they are able to see somebody,” Simms explained. “It helps us keep an eye on our patients. Due to the restrictions that have been loosened for healthcare in general right now if the patient has a smartphone we’re able to FaceTime with them.”
Being unable to get out to doctor appointments can cause a sense of panic. Simms understands that.
“We’re also trying to drive down the fear with our patients because we’re trained and we know how this process works,” Simms said. “We’re not scared and know how to take care of you. There’s a lot of fear circling. We have to be the forefront of education.”
Being able to talk to patients in their own home at their own pace is an invaluable piece of the puzzle. Simms said Interim providers are able to have those conversations that rely on facts not the latest headlines.
“I believe we do an excellent job during this scary time,” Simms said. “At the top, it’s important we support our nurses. I think being the calm in the storm is what we do best. Before Covid, we took high-risk patients.”
“Because that’s already our platform, Covid was just a step up for us. We’re able to educate why (a patient) might be at more risk. We’re able to take that time, take those precautions and provide that education.”
Interim is locally owned and part of a national network of more than 300 offices.
Employing more than 75,000 healthcare workers, Interim provides care to more than 50,000 patients each day.
Simms explained Interim revolves around key concepts including: preparation and training, monitoring and reporting, alternative methods of care, high standards of safety and an emergency preparedness plan.
And in these trying times, Simms said Interim has made it a greater focus to love on its frontline staff.
From lunches and breakfasts to special personal protective equipment including floor mats and car seat covers, Interim is protecting those who protect us all.
“At Interim we believe we are all in this together and I think being the calm in the storm is what we do best.”










